| [1] |
Lian-Shun Feng. Development and Advances of Drugs for Cancer Theranostics – PART-IV[J]. Current Topics in Medicinal Chemistry, 2021, 18(21): 1644.
|
| [2] |
Tosca E. M, Ronchi D, Facciolo D, et al. Replacement, Reduction and Refinement of Animal Experiments in Anticancer Drug Development: The Contribution of 3D In Vitro Cancer Models in the Drug Efficacy Assessment[J]. Biomedicines, 2023, 11: 1058. doi: 10.3390/biomedicines11041058
|
| [3] |
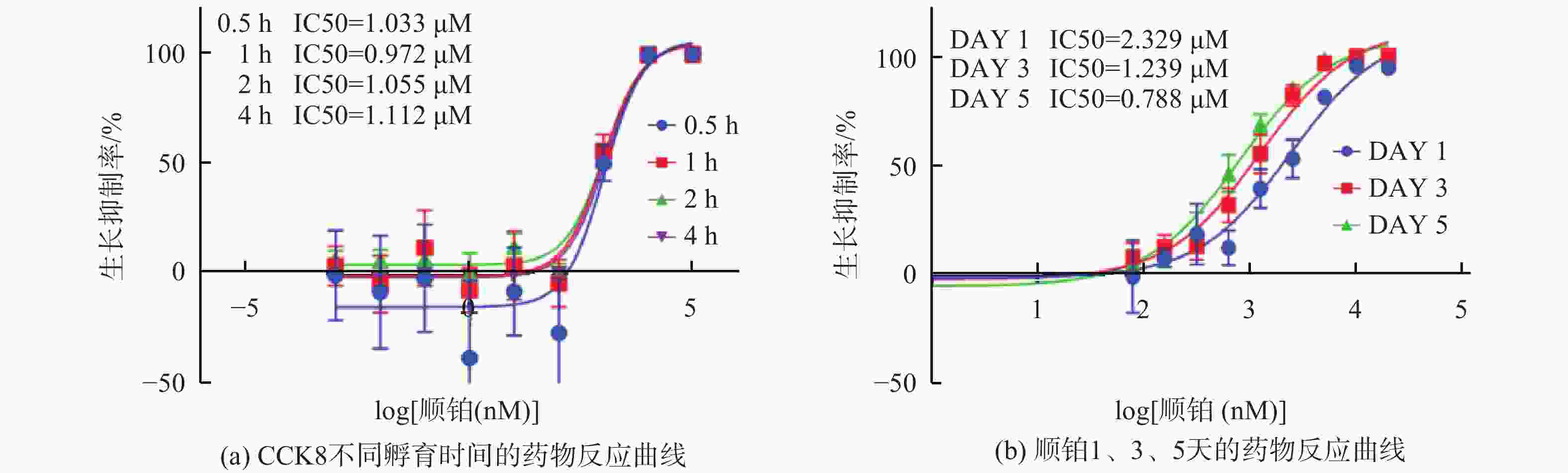
薛志超, 赵佳威, 李永淑, 等. 细胞密度对抗癌药药效评估准确性的研究[J]. 计量科学与技术, 2023, 67(4): 57-62,56.
|
| [4] |
Jaroch K, Jaroch A, Bojko B. Cell cultures in drug discovery and development: The need of reliable in vitro-in vivo extrapolation for pharmacodynamics and pharmacokinetics assessment[J]. Journal of Pharmaceutical and Biomedical Analysis, 2018, 147: 297-312. doi: 10.1016/j.jpba.2017.07.023
|
| [5] |
Schilling K, Harris AL, Halliday AN, et al. Investigations on Zinc Isotope Fractionation in Breast Cancer Tissue Using in vitro Cell Culture Uptake-Efflux Experiments[J]. Front. Med, 2022, 8: 746532. doi: 10.3389/fmed.2021.746532
|
| [6] |
Faruqui Nilofar, Kummrow Andreas, Fu Boqiang, et al. Cellular Metrology: Scoping for a Value Proposition in Extra- and Intracellular Measurements[J]. Frontiers in Bioengineering and Biotechnology, 2020, 7: 456. doi: 10.3389/fbioe.2019.00456
|
| [7] |
Mirabelli, Coppola, Salvatore. Cancer Cell Lines Are Useful Model Systems for Medical Research[J]. Cancers, 2019, 11(8): 1098. doi: 10.3390/cancers11081098
|
| [8] |
薛志超, 曾嘉明, 李永淑, 等. 接种数量对细胞生长和药物作用的影响及细胞计数方法对比[J]. 计量学报, 2023, 3(44): 341-349.
|
| [9] |
Minerva, Amrita Bhat, Sonali Verma, et al. Cisplatin-based combination therapy for cancer[J]. Journal of Cancer Research and Therapeutics, 2023, 19(3): 530-536. doi: 10.4103/jcrt.jcrt_792_22
|
| [10] |
Raudenska Martin, Balvan Jan, Fojtu Michaela, et al. Unexpected therapeutic effects of cisplatin.[J]. Metallomics, 2019, 11(7): 1182-1199. doi: 10.1039/c9mt00049f
|
| [11] |
Mengdi Song, Mingxiao Cui, Kehai Liu. Therapeutic strategies to overcome cisplatin resistance in ovarian cancer[J]. European Journal of Medicinal Chemistry, 2022, 232: 114205. doi: 10.1016/j.ejmech.2022.114205
|
| [12] |
Chenying Jiang, Chenjun Shen, Maowei Ni, et al. Molecular mechanisms of cisplatin resistance in ovarian cancer[J]. Genes & Diseases, 2023, 1: 1.
|
| [13] |
Liang C, Zhang Hy, Wang Yq, et al. TMED2 Induces Cisplatin Resistance in Breast Cancer via Targeting the KEAP1-Nrf2 Pathway[J]. CURR MED SCI, 2023, 43: 1023-1032. doi: 10.1007/s11596-023-2777-7
|
| [14] |
alma Y Mohamed, Hisham A Elshoky, Nayera M El-Sayed, et al. Ameliorative effect of zinc oxide-chitosan conjugates on the anticancer activity of cisplatin: Approach for breast cancer treatment[J]. International Journal of Biological Macromolecules, 2023, 257: 128597.
|
| [15] |
A Rane, J Jarmoshti, A Siddique, et al. Dielectrophoretic enrichment of live chemo-resistant circulating-like pancreatic cancer cells from media of drug-treated adherent cultures of solid tumors[J]. Lab Chip, 2023, 6: 10.
|
| [16] |
Grela E, Kozłowska J, Grabowiecka A. Current methodology of MTT assay in bacteria – A review[J]. Acta Histochemica, 2018, 120(4): 303-311. doi: 10.1016/j.acthis.2018.03.007
|
| [17] |
Ludmil Benov. Improved Formazan Dissolution for Bacterial MTT Assay[J]. Microbiology Spectrum, 2021, 9(3): 1.
|
| [18] |
Yanfeng Zhu, Weihui Chen, Weiqun Guan, et al. Study of As2O3 regulating proliferation and apoptosis of Tca8113 cells by inhibiting the expression of Id-1, Artificial Cells[J]. Nanomedicine, and Biotechnology, 2019, 47(1): 1932-1937.
|
| [19] |
Jun Wang , Wei Lei, Gang Li, et al. CD151 promotes proliferation and migration of SK-NEP-1 cells via the GSK-3β/P21/cyclinD signaling pathway[J]. Pathlogy-Research and Practice, 2019, 215(2): 329-334.
|
| [20] |
Ling Cai, Xijiang Qin, Zhihui Xu, et al. Comparison of Cytotoxicity Evaluation of Anticancer Drugs between Real-Time Cell Analysis and CCK-8 Method[J]. ACS Omega, 2019, 4: 12036-12042. doi: 10.1021/acsomega.9b01142
|
| [21] |
Jing-Ru Song, Na Li, Dian-Peng Li. Synthesis and anti-proliferation activity of mogrol derivatives bearing quinoline and triazole moieties[J]. Bioorganic & amp; Medicinal Chemistry Letters, 2021, 42: 128090.
|
| [22] |
de la Fuente-Jiménez J L, Rodríguez-Rivas C I, Mitre-Aguilar I B, et al. A Comparative and Critical Analysis for In Vitro Cytotoxic Evaluation of Magneto-Crystalline Zinc Ferrite Nanoparticles Using MTT, Crystal Violet, LDH, and Apoptosis Assay[J]. Mol. Sci, 2023, 24: 12860. doi: 10.3390/ijms241612860
|
| [23] |
Magdalena Boncler, Marek Różalski, Urszula Krajewska, et al. Comparison of PrestoBlue and MTT assays of cellular viability in the assessment of anti-proliferative effects of plant extracts on human endothe[J]. Journal of Pharmacological and Toxicological Methodslial cells, 2014, 69(1): 9-16. doi: 10.1016/j.vascn.2013.09.003
|
| [24] |
Kumar Priti, Nagarajan Arvindhan, Uchil Pradeep D. Analysis of Cell Viability by the MTT Assay[J]. Cold Spring Harbor Protocols, 2018, 6: 469-472.
|
| [25] |
Yu C, Zhang X, Wang M, et al. Afatinib combined with anti-PD1 enhances immunotherapy of hepatocellular carcinoma via ERBB2/ STAT3/PD-L1 signaling[J]. Front Oncol, 2023, 13: 1198118. doi: 10.3389/fonc.2023.1198118
|
| [26] |
Wang Junbin, Gao Jin, Chen Qinnan, et al. LncRNA LINC01116 Contributes to Cisplatin Resistance in Lung Adenocarcinoma[J]. OncoTargets and Therapy, 2020, 13: 9333-9348. doi: 10.2147/OTT.S244879
|
| [27] |
anfang Wang, Zhenhao Zhang, Wei Wan, et al. FAM19A5/S1PR1 signaling pathway regulates the viability and proliferation of mantle cell lymphoma[J]. Journal of Receptors and Signal Transduction, 2022, 42(3): 225-229. doi: 10.1080/10799893.2021.1895220
|
| [28] |
Wang Ya, Zhang Xiaomei, Zhao Boyuan, et al. Suspension State Promotes Drug Resistance of Breast Tumor Cells by Inducing ABCC3 Overexpression[J]. Applied Biochemistry and Biotechnology, 2020, 190: 410-422. doi: 10.1007/s12010-019-03084-0
|
| [29] |
Mao Yuqiang, Yu Ying, Han Yun. Influence of thoracic drainage fluid on proliferation, migration, apoptosis, and drug resistance in lung cancer cell lines[J]. Cancer Management and Research, 2019, 11: 2253-2259. doi: 10.2147/CMAR.S187019
|
| [30] |
Zhuo-Ya DAI, Shuang-Mei JIN, Hong-Qin LUO, et al. LncRNA HOTAIR regulates anoikis-resistance capacity and spheroid formation of ovarian cancer cells by recruiting EZH2 and influencing H3K27 methylation[J]. Neoplasma, 2021, 68(3): 509-518. doi: 10.4149/neo_2021_201112N1212
|
| [31] |
Grimes D R, Fletcher A G. Close Encounters of the Cell Kind: The Impact of Contact Inhibition on Tumour Growth and Cancer Models[J]. Bulletin of Mathematical Biology, 2020, 82(2): 20. doi: 10.1007/s11538-019-00677-y
|


 作者投稿
作者投稿 专家审稿
专家审稿 编辑办公
编辑办公

 下载:
下载: